While Canada has achieved universal public healthcare coverage, that does not mean conservative forces have given up trying to erode that coverage and expand corporate care where it does not currently exist. The battle has become particularly intense in Ontario under the Ford Progressive Conservative government, which is implementing serious cuts to the level of care and moving to bring in for-profit mini-hospitals.
Inadequate Staffing. Less and less of hospital spending is on staff. Employee compensation as a share of hospital expenditures has consistently shrunk in Ontario.
This is not some immutable law of hospital development. It is in stark contrast with the rest of Canada, where compensation has become a larger share and now accounts for 67.1%.
Hospitals in provinces other than Ontario now have 18 percent more staff per capita than hospitals in Ontario.

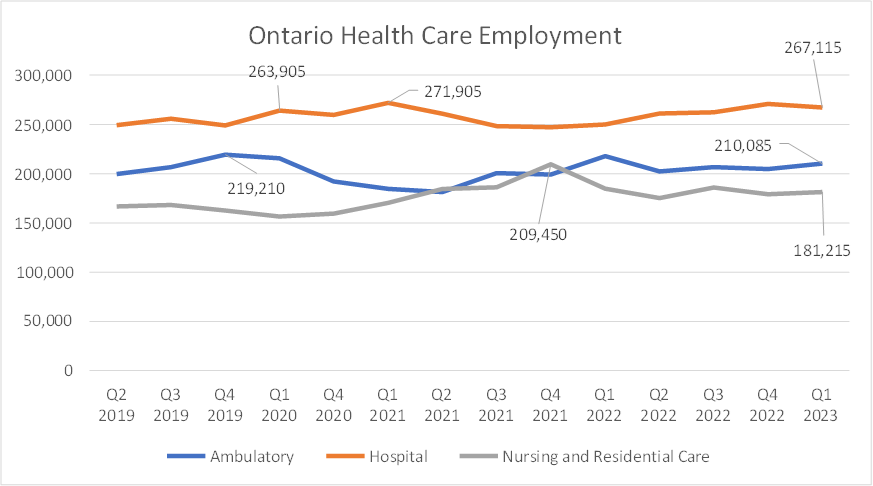
All three health care subsectors are down from previous highs in employment.
The shortage of hospital workers: With deteriorating working conditions, hospital job vacancies have grown dramatically. There are over three times the number of hospital job vacancies in the first quarter of 2023 than in 2015.
Consequences of the Staffing and Capacity Crisis: Most notably, emergency rooms have closed hundreds of times in 2022 and 2023. Unplanned closures of ERs is a new situation, almost never seen before.
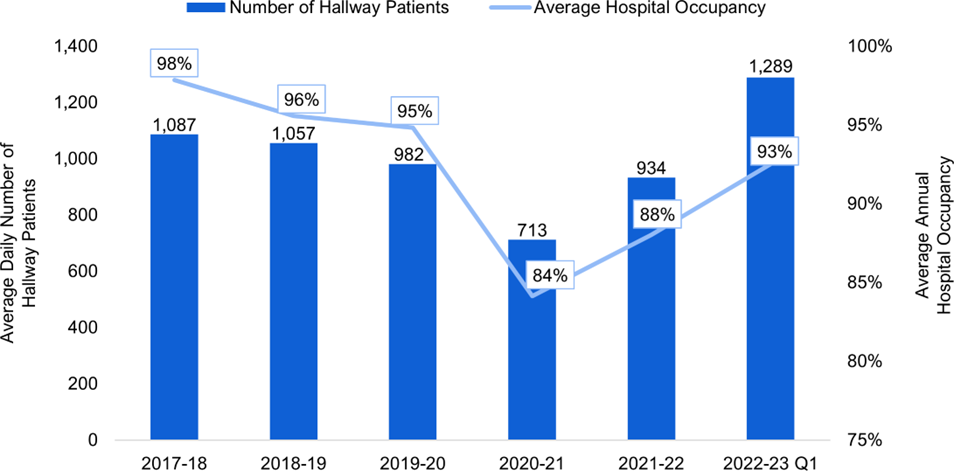
In 2018, the Progressive Conservatives ran on a promise of ending hospital hallway healthcare. In fact, the problem has gotten worse. The number of inpatients being cared for in hallways has hit 1,289 per day an all-time high, 22% higher than when the government was elected in June 2018.
Surgical wait times in 2022 were 49 percent longer than 2019.
The government treats these nominal increases as if they are improving service levels. Measured against need, however, Ontario is facing a sharp decrease in service levels.
That nominal increase won’t come even close to covering off increasing demand for services due to population growth, which according to provincial government projections, will be about 15%. The demands on health care will be much more than this, however, due to a rapidly aging population.
Health care needs are very sensitive to age.

People 65 years of age or older use most of our hospital bed days -- 59.5% hospital bed days in 2021/22.
The population of the 65+ age group is currently growing according to Ontario Ministry of Finance data by more than 3% a year, twice the rate of the overall population. We will have about a third more people aged 65+ in a decade. The total 65+ age group is projected to grow by 63 percent by 2046 (from 2.7 million to 4.4 million), but the 75+ group will increase 125%, and the 90+ age group will increase 213%. The very rapid growth of these latter two age groups will drive up demand even more quickly.
Government plans for the years immediately ahead are even worse. The FAO reports that only 1,000 new beds will be added in the next four years, less than a 3% increase. That four-year increase is enough for about two years of population growth, with nothing to offset aging, much less improve service levels to deal with the capacity crisis.
The rapid growth in the number of elders is driving up the need for hospital beds (and the hospital workers to staff them) by more than triple the planned increase in staffed beds.
The plan, however, is to double down on long-term cuts in hospital service levels.
Amid a hospital capacity crisis, the plan is to reduce hospital capacity relative to need.Home care: The government trumpets new money for home care - -but (with aging and population growth) the FAO projects a decline in the number of nursing and personal support hours per Ontarian aged 65 and over, from 20.6 hours in 2019-20 to 19.4 hours in 2025-26. That is down 5.8% -- almost 1% per year. There is no relief planned through home care - - in fact just the opposite.
Long-Term Care: The FAO now sees a slight improvement in the ratio of long-term care bed to elders 75 years of age and over -- from 71.3 beds per 1,000 in 2019-20 to 72.1 in 2027-28. The increase amounts to a 1.1% increase over 8 years. That's an increase of 0.1% per year.
This tiny increase is the plan when almost 40,000 elders are on the LTC wait list and the government has just passed legislation to require hospital patients to move into long-term care more quickly.
Even with this very modest increase, we are still far short of the 90 beds per 1000 elders 75+ in 2010/11 -- 20% less. As with home care, there is no relief coming from the current plan for LTC development.
The Fake Solution: For-Profit Care: In 2022/23, hospital funding was cut by $156 million. For this year, budgeted funding for hospitals was $23,773,093,800, an increase of $115,458,800 or 0.488% over the 2022/23 Budget Estimates (of $23,657,635,000).
In contrast, so called “Independent Health Facilities” (i.e., private, for-profit surgical and diagnostic facilities) are budgeted to get a 212% increase from last year’s Budget Estimates. As shown in the 2022/3 and 2023/4 Estimates, IHF budgeted funding increased from $38,693,100 to $120,693,100. That is an increase of exactly $82 million – or 211.92%. In dollar terms, they budgeted almost as much of an increase to the tiny IHF sector ($82 M) as they did for the entire public hospital system ($115.5 M). It is a boom for private profits, even as the government implements harsh austerity for public hospitals.
Yet this is where the government has chosen to focus its energies in the midst of a severe capacity crisis. This is, at best, an attempt at a diversion from the need to develop more capacity. True solutions lie elsewhere.
Health care capacity is in crisis now, service levels have declined and the plan is to reduce capacity further. This fits with the attacks on living standards via housing and inflation, reducing living standards now at a faster rate than we have seen for many decades. Capitalist rule is not delivering. Change is required.






Comments
Post a Comment