Lost time injury (LTI) claims for workers compensation by health care support workers have shot up in the last few years, even before COVID-19.
For many years, claims were in the 2,500 range, before starting an upward track in 2014, rising to 4,271 in 2019, just before COVID-19 hit. That is about a 60% increase. Other major occupations
in health care saw the number of claims remain basically flat between 2002 and 2019 (with things changing in 2020, as we shall see).
By 2019, health care support workers had the second most workplace lost time injury claims of any occupation reported by the Workplace Safety and Insurance Board (WSIB) - only motor vehicle and transit drivers had more, with 4,901 in 2019. In 2002, health care support workers had only the eighth highest number of LTI claims. So things have changed.
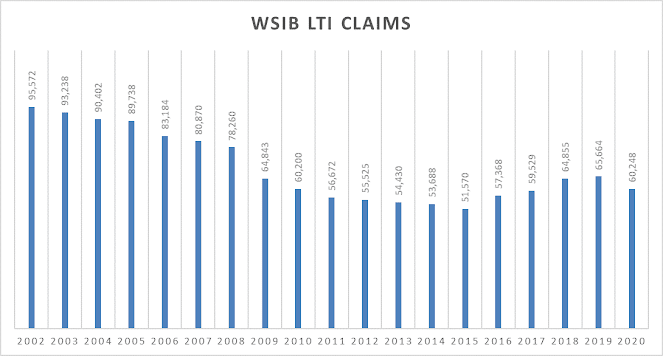
The increase in injury claims among health care support workers is more remarkable as WSIB has been on a tear to reduce lost time injury benefit claims – with total claims for all occupations falling from 95,572 in 2002 to 65,664 in 2019, a 31% reduction, even as the workforce grew. (This laid the basis for major WSIB premium cuts for employers since 2015, including $1.45 billion in 2019. Current plans are to cut employer premiums by billions more.)
The result is that health care support worker LTI claims became a much larger share of the total claims, increasing from just over 2% of all claims in the early 2000s to just over 6% in 2019. Notably, health care support workers have accounted for the most female LTI claims since 2006.
 |
The explosion of health care claims after COVID: LTI claims for health care support workers increased from 4,271 claims in 2019 to 7,850 claims in 2020[1]. That is an 84% one-year increase in LTI claims. As a share of all LTI claims, health care support workers accounted for 6.5% of all claims in 2019, but 13% in 2020.
The number of LTI claims by health care support workers was by far the highest of any other occpation reported in 2020 - - well more than double the occupation with the second most number of LTI claims.
The other major categories of health care occupations also saw a major increase in LTI claims in 2020, with RN (and nurse supervisor) LTI claims increasing from 1,378 to 2,433. That is a 76.5% increase, not quite as big as the increase in health care support worker LTI claims but quite remarkable nonethless. “Technical and skilled” occupations in health care increased from 2,198 claims to 3,630 claims, a 65% increase.
The increase in health care worker claims in 2020 was driven, of course, by COVID-19. WSIB reports 12,768 COVID-19 LTI claims in 2020, fully 21.2% of all LTI claims.
[1] Although WSIB refers to the year as
“2020”, it actually reports LTI on the basis of the fiscal year April 1 -March
31, so “2020” closely fits the first year of the COVID-19 pandemic.

Comments
Post a Comment